Overview
In this next episode I was honored to be joined once again by Michael Guirguis, M.D. He is currently a practicing emergency medical physician, a Medical Director for an ultra high net worth family office, he supports the San Bernardino County Sheriff’s as a Deputy Flight Physician, and he’s also a contributor to the Board of Executive Protection Professionals. In terms of education, he’s a graduate of Harvard Medical School, UCLA, and also a Loma Linda Medical Center post-grad.
Today’s discussion gets away from the normal format of the show to focus on one topic specifically: medical kits.
How should we think about the medical kits that we build? How should we pack them? What are common mistakes? Plus, for the last 25 min of the show, Dr. Guirguis critiques my medical bag and gives me considerations for improving it.
—–
Big Ideas from This Episode
- First, consider your mission. You need a bag that fits the purpose (e.g. covert vs overt; lots of molle straps is not covert).
- Keep PPE immediately available on the outside of the kit so they are easily accessible.
- “Stack your bag the way you’re going to do your assessments!” (e.g. your PPE, your tourniquet, and your hemostatic gauze, etc should be at the top of the bag to immediately address a massive hemorrhage (“M”))
- Have a single way that you approach every patient assessment (e.g. ABCDE, MARCH PAWS, etc.). Get really good at using that algorithm.
- Using something like a blood pressure cuff is basically overkill when doing your initial assessment because a simple manual check of the patient’s pulse provides indicators about pulse and blood pressure.
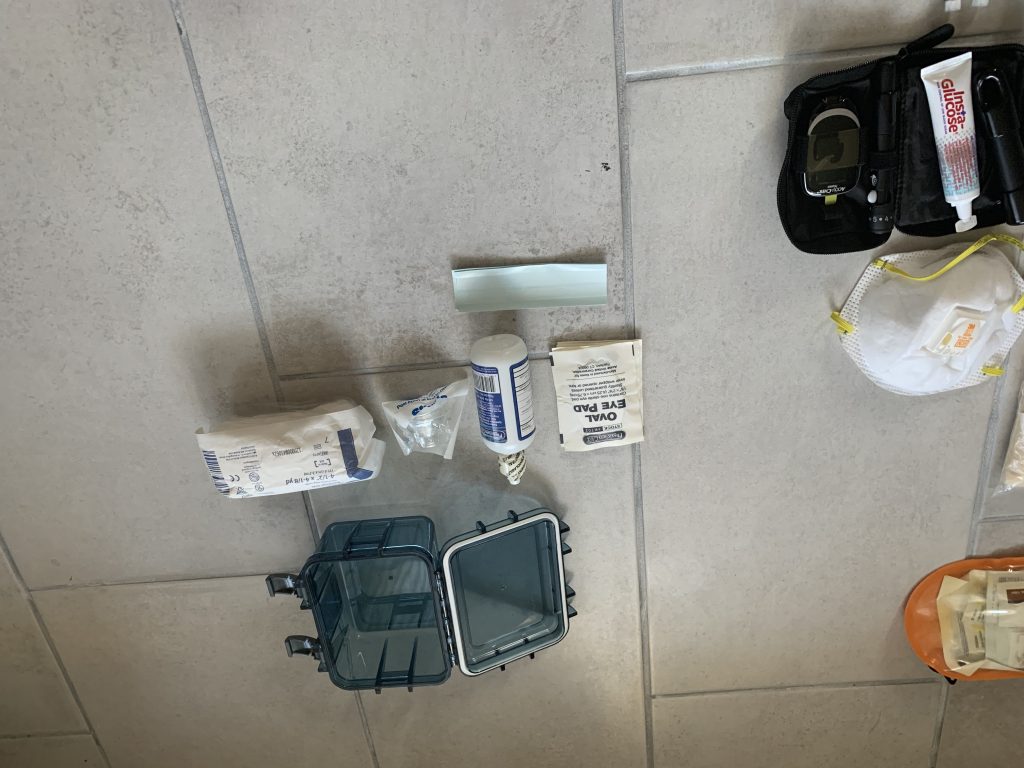
CRITIQUE OF MY MEDICAL BAG (Pics/Itemized list)



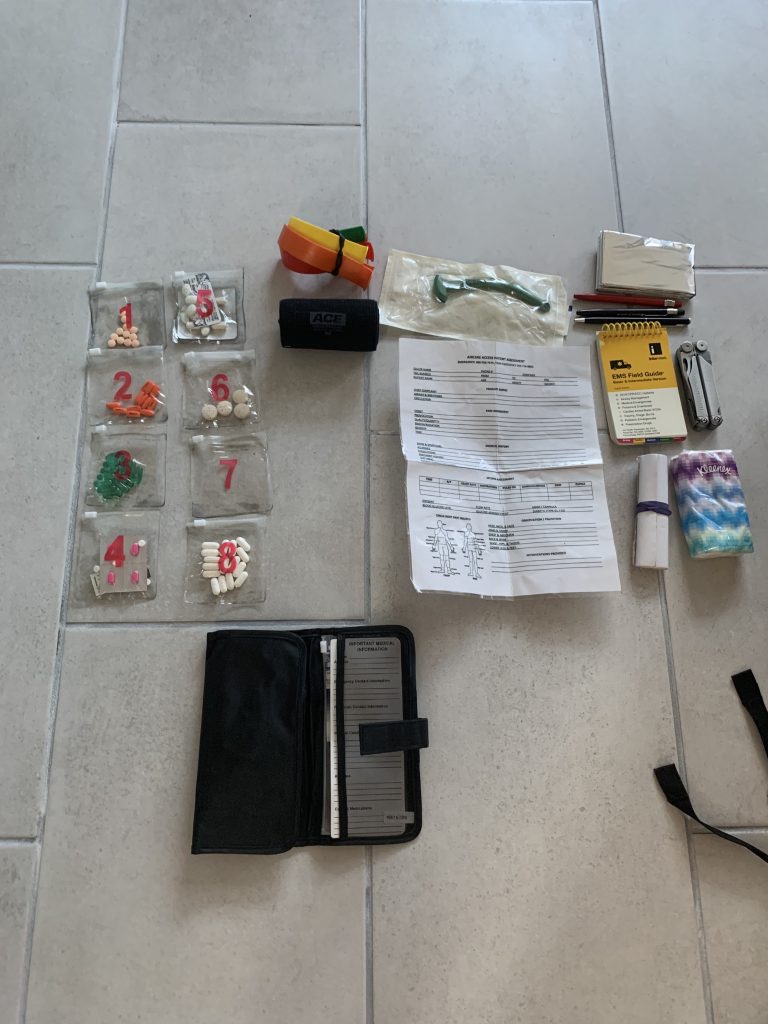



IMPROVEMENTS MADE POST-CRITIQUE
I got rid of these items:
- Replaced all loose over the counter medications with individual, travel size servings.
- Electronic, forehead thermometer
- C-Collar (rationale: it takes up a lot of space and if the C-collar is necessary then you probably also need a backboard)
- Splinter out
- Electrical tape and full roll of gorilla tape (rationale…keep a slimmed down role of duct tape, which can be small and rolled around a small item)
- EMS field guide (use an app based one if needed)
- Pupil light (use phone instead)
I added these items:
- Itemized list of bag’s contents for conducting future inventories
- Soft-T tourniquet
- Pulse oximeter
- Epipen (carrying for a loved one, not for my personal use)
- *If I can get my hands on it, I’ll replace crazy glue with derma bond
- Extra pair of nitrile gloves
I replaced these items:
- Replaced all loose over the counter medications with individual, travel size servings.
- Replaced electrical tape and full roll of gorilla tape (rationale: too much tape, keep a slimmed down role of duct tape such as several feet rolled up)
- Replaced EMS field guide with an app based alternative
- Replaced manual BP cuff for automatic one
Use CONTROL + F to search the transcript below if you want to learn more!
Transcript from this episode (#17)
*Note: this transcript was generated using automated software, and my not be a perfect transcription. But I hope you find it useful.
Travis 0:00 ... Michael, thank you for joining me on the podcast again today. So today's episode is special, because you're here to chat about a unique topic, which is medical bags and medical kits. And to make our conversation even more relatable, or as relatable as possible for listeners, part of the conversation today is going to be you critiquing the medical bag that I've sent over to you. So I send you over a list of pictures and kind of like an itemized list. And all of this is also available on the show notes. So people can dive in there and get a little more context about the medical bags and the medical bag and the items that we're talking about. And for context, the purpose of this bag that we're going to be talking about a little bit today was basically to be like a backup when I was working in Eep, meaning if I was ever out with one of the secondary principals or maybe the principal's friends, or whoever was not the primary principal, that I'd still have a bag available so that I can provide like a minimum level of care if if EMS was not reachable immediately, and let's see. So that's the context. And I'm certainly a novice when it comes to emergency medicine, as you know. So previously, I earned my EMT license, I've taken some similar courses. But as far as things go today, in my day to day and security, I'm very much not focused on emergency medicine. I'm actually focused on physical security and doing assessments when it comes to technology and hardware, and all that fun stuff. So Michael, thank you very much for joining me. Michael 3:21 Thank you, Travis, for having me. Again, I'm looking forward to you know, this stock. I think like most people, they're in the security industry, they're the medicine background is, is probably not the strongest point for them. And you know, I think that's the point of this podcast is just kind of discuss, discuss it and figure out what what we need to carry and you know, what we can use the to be the most helpful to our clients. Travis 3:46 Yeah, I think a couple big takeaways, I think the biggest thing that people could take away from our conversation today, I think there will there will definitely be like a handful of small aha moments when we talk about, especially the way that you kind of conceptualize in the way that you think about emergency medicine and the way that you think about prioritizing different items and different measures. So I think, I think if there's one big thing, people will take away a handful of those moments. So to kick things off, I wanted to ask you, so what are your thoughts on medical on bags for carrying medical gear? And maybe how does this one that we're talking about today fit your general preferences? Michael 4:27 So I think for you know, the type of bag you're carrying the size of the bag you're carrying, it all depends on the mission. So the bag that you've showed me, I liked that bag, it's a very nondescript, it's a non you know, 511 type Molly strap bag that you could spot from a mile away that looks military. So for this bag, that'd be great for like a coke protein. Or if you're, you know, walking into a hotel with a client, you know, you couldn't tell if that's just a backpack full of clothes. or, you know, what it's used for, which is all medical gear, multiple straps on the outside. And my big thing is, you know, keep your PPE your gloves, maybe a small mask, I mean, in this day and age, you could probably just walk around with a mask, but nobody would even think, you know, think twice about it, but just keep your PPE on the outside. So if something does happen, it's either in your pockets, or it's easily accessible in your backpack. You know, for other things, these medical bags, they all range, right. So I mean, you can have like an IFAK, which is very small, you know, on your person, you can have, you know, this is kind of a mid size backpack type, bag, and that goes all the way to, you know, vehicle med kits, all the way to, you know, multiple large bags with medical equipment, if you're going, you know, somewhere international or, you know, somewhere rural, where you want to have a more advanced kit. So I think, you know, so you know, this is a perfect COVPRO bag, it's a perfect bag to be around the city, let's say if you're gonna go somewhere more rural, you may want to have a, you know, this bag along with more advanced medical equipment, or heavy equipment or large equipment that's actually in a car kit that you're not having to carry. And then as you go, let's say the client wants to travel internationally, then you're gonna have even larger kits, and you may add medications, antibiotics and other things, depending on which area of the world you're going to what endemic disease is in that area. And you can kind of tailor your bags to that. Travis 6:40 Cool. Yeah, I like that way of thinking. And that's essentially kind of like, what the purpose of the bag was, it was more for something that can be easily thrown into a vehicle. And then when you stop somewhere, you can easily just take a ride out, not necessarily like one of the big comprehensive ones that you're pretty much always going to leave with the primary vehicle. Yeah, so I was gonna say and one thing also. So as I started putting together this list, like this itemized list of all the items in the medical bag, and really dumping everything out and taking a close look at everything. I also noticed like I also made some of my own, like mistakes or some of my own, like poor assumptions. For example, as I was going through this kit, one more time, before the show, I realized one that I had taken out some of my some of those items and put them in the bag, and that goes in my truck. So like, I thought that I had a pulse ox in there. And I thought that I had a backup like a soft T winless tourniquet. So I noticed like some simple errors like that. So that also kind of goes back to a point that you made on a previous podcast, which was that you really need to know your bag and empty it out every once in a while and go through everything. And then another another big issue that I noticed with my bag two, and I think we'll probably get into it a little later. But when it came to my over the counter medications that I had, some of them were unlabeled, and I just completely forgot what they were. So yeah, those are like some simple mistakes that any of us can make. And it just gets back to us knowing being like, having intimate knowledge of everything that's in our bag, and where it's placed. And just knowing everything about our bag. So now moving on, I wanted to ask you, so I know you have like a very unique expert way of looking at medical gear and kind of categorizing it in in your mind. So can you tell me how you think about medical gear when it comes to the types of items and interventions? Like some of the different ways that you think about it? Michael 8:49 Yeah, so for me for you know, when I carry medical gear, it depends on you know, my mission, you know, I fly Air Rescue, you know, we've got medical gears set up, but then I also carry my own medical gear, you know, things that I like to use that may not be in the team bags. So one thing is kind of your mission. The other thing is just having a a way you assess people so unlike T Triple C they teach, you know the march on us, for me, I just use a simple ABCs of Emergency Medicine, you know, the March algorithm is more for trauma. For me, I use the ABCs which is just more for anything. And I can kind of discuss how I will assess someone via the ABC approach versus the march pause. And so for us, for those listeners who don't know with you know, the March algorithm is it's you know, the M is massive hemorrhage. You control that then you move on to a the airway, and then three respirations. Once you've got airway and respirations, either by bagging or if there's nothing wrong with it, you move on to see circulation. Ah, you're going to be dealing with hypothermia and heading injury. And then the pause part is, after that initial offset assessment, that's kind of like my secondary assessment that I'll do, you know, you kind of cover all life threatening things in that primary assessment. And then you move on to the P of pauses pain management, antibiotics, wounds, and then splinting and so that's a teacher pool. See thing because, you know, domestically here, we're not giving antibiotics in the field, like you would do in the military, where you're probably not as close to, you know, higher level Medical Center, and where there's open trauma and things you want, you want to get antibiotics on board to prevent, you know, sepsis and septic shock later. So, you know, in terms of the ABCs, so for me, it's, if there's trauma, I always kind of in the back of my mind, I just add hemorrhage if I if I walk up on a patient or if a patient comes into my emergency department, or if I'm in the field, if they're obviously bleeding from somewhere, I assess is it you know, massive hemorrhage? Or is this just like a little small nicking cut, if it's a massive hemorrhage, I have to stop it. And we stop it with you know, all the tools that you learn in T, Triple C, you know, it's either a pressure bandage, pack, the wound, tourniquets, direct pressure, you kind of stop that, and then we can discuss kind of more as we go on. And then from there, it's it's airway for me. So you know, is that patient person breathing? Is there something in the airway? Do they have facial injury, whether aspirating blood? Do they need, ET tube? Do they need some simple as just maybe a nasal pharyngeal airway? What's basically for those who may not know it's just a little tube that goes into your, your nose and into the back of your throat to help open up your airway? Or do they just need a simple maneuver like a chin lift jaw thrust? So do you if they're laying on their back? Do you just put their chin up to the sky and put your fingers behind their jaw, just move it up towards the sky, just kind of bring that tongue instead of it laying back in the mouth, just bring it upwards, and that helps open up, you know, the airway. And please interrupt me because I don't want to just keep talking through my whole assessment. So you know, at that point, you know, it's something simple like a maneuver like the chin lift jaw thrust, or it's even more simple. They don't have an airway issue at all. You walk up to them, they're talking to you, and they look like they're not in any respiratory distress. Maybe they've just got an extremity injury, and you've already passed airway, and you're moving on to breathing, you know, the breathing is is are they spontaneously breathing? If they're talking to you, and they're no distress, and they're not, you know, breathing 3040 50 times a minute, you know, you're moving on. If they are in distress, do you need to do mouth to mouth? Better yet? Do you have a bag valve mask? Where you can, you know, help augment their breathing? Do they have a reason to be short of breath? Did they take an injury to their chest? Do they have penetrating trauma? Do they have blunt trauma? Do they have, you know, broken ribs and flail chest, you know, and if they've got any of those things, you're just going to address them like you would learn in T Triple C by placing chest seals, all the way to if they have a tension pneumothorax and you're you've been trained domestically, if you're a paramedic, and above with more training, then you've probably been trained how to do a needle thoracotomy. And you can do that for you know, not just pneumothorax but a tension pneumothorax you know, to prevent cariogenic shock, and basically respiratory arrest. Travis 13:37 And hey, Michael, can I stop your sec, just to ask you a little more. So, can you explain a little bit about how the chest seal works when someone uses that Michael 13:47 they call it a sucking chest room. So basically what happens is, is if you take an injury to the chest wall, and then you have to realize that the chest wall and the lungs, you know, when you're in full inhalation your diaphragm, which basically sucks down during inhalation, when you're taking a deep breath can pretty much go down to your belly button. So depending on when you take an injury, if someone's in full inhalation and they've got a gunshot wound or a stab wound above their belly button, they technically could have, you know, a pneumothorax it may have hit actual lung. And what will happen is is as you make that hole there's a negative pressure so when your lung expands, it sucks air in from the hole and your holes are your mouth and your nose. If everybody were to go home and X you know completely exhale. And then take your hands, pinch your nose and cover your mouth and try to inhale. You can't do it. You physically cannot take a deep breath. If you're pinching your nose, holding your mouth and then try to inhale. You can't do it because there's a negative pressure that's set up in your chest cavity and the only way that air can get in is through your nose and mouth. Unless you've got a penetrating injury, so now if you hold your nose in your mouth, but you have a big hole in your chest from around or shrapnel or metal or whatever, you know, now that air can get sucked in through that hole in your chest. And what happens is between your lung and your chest wall, there's what's called a pleural space. And there shouldn't be any air in between that pleural space, it's just kind of negative air when your lung expands and retracts. While the problem is, is if you've got that hole in your chest, you can actually get air in the hole and your, your chest wall acts like a one way valve. So the air will suck in between the lung and the chest cavity. And every breath you take, it just sucks and more air sucks and more air to the point where that air can't get released. And your lung just keeps collapsing, collapsing collapsing towards your heart collapsing collapsing to the point where it actually there's so much pressure between the chest wall and the lung, that it's actually pushing now, your heart and your aorta to one side or the other. Basically just kicking off the order. And when that happens, that's how you're going to, you know, cardiac, cardiac arrest, your hearts no longer able to pump because the outlet and the inlet have been kicked off from that pneumothorax. So that's where you put the needle in. You know, the theory is, is it's not the theory. I mean, basically, the pathophysiology is, you've got that air that can't go out and it's under such high pressure, it's pushing the heart over, you can dark that chest, you pull your catheter out, you've got now hollow needle in the chest, and there's such high pressure that the air just comes whooshing out. That being said, it's only good for, you know, certain amount of time. So what you need to do is cover that chest seal. So basically, like you're taking your hand over your mouth and your nose and not allowing air to come in, if you can put that you know, wipe the blood down, put the plastic chest seal in, it will no longer allow air to enter that chest wall. Because of that plastic dandy pretty much over the over the hole in your chest. Travis 17:03 I see. Yeah, thank you for all these analogies, this is a really good explanation of how using the thoracotomy needle goes hand in hand with the chest seals and how those interact with each other. But like when, of course, like when you have the very unique situation to use to use them together. That's very interesting. Michael 17:24 Real quick, a lot of this, if you can understand the concepts, it just makes it a lot easier to understand what you're doing, you know, your, your body is an amazing thing. But it's you know, it's it's plumbing and it's electrical. I mean, if you're a plumber, you're an electrician. That's how the body works, right? It's electrical signals from from the brain plumbing, which is your cardiovascular system. And if you can kind of understand basic plumbing, electrical concepts, it's pretty much what the body is. So you don't have to overthink it or let it just kind of, you know, it's medicine. It's difficult. It's not, it's really just simple. If you can just get the step by step of what is happening. It's very easy to just say hole, cover it up. So you don't you know, you can prevent a tension pneumothorax. Travis 18:14 I see. And then I kind of interrupted you a little bit. So I think you were going on, you talked about airway, breathing circulation. Michael 18:23 Yeah. And I think we're done with airway and breathing is now it's just circulation. So once you basically manage the airway, you've, you're helping them breathe, or they don't have a breathing issue, then you you look at circulation, right. So obviously, we stopped any hemorrhage into trauma, we stopped hemorrhage. So that's fine. Now it's just a matter of do they have pulses, right? That's the best way to check circulation? Do you need to do CPR? Do they have a radial pulse? You know, we can talk about some of the equipment you have. I mean, you've got a stethoscope and a beak, BP cuff. But just in terms of me, I'm just looking for pulses, right? If they've got a radial pulse, their blood pressure is at least 80 systolic right? If they don't have radial pulse, you know, then I can go to maybe the femoral artery in the groin checked out. If they have that, then their blood pressure is at least 70 just a rough estimate, if they don't have a femoral pulse, then you go to carotid. So I think you know, the big thing is, you know, in CPR today, they asked you to check for carotid one, it's pretty easy. You don't have to dress anybody or you know, feel through clothes and jeans. But if you don't have a carotid pulse, that means your your heart rate is less than 60. And you know, the teaching is start CPR. So that's a very simple way without having to do an act of blood pressure. Now there's a role in having a blood pressure cuff and getting a real blood pressure. I mean, there's a big difference between someone who's got a 90 over, you know, 50 heart rate with a radial pulse and someone who's got a 150 over, you know, 80 you know, blood pressure. So, you know, there is a role for that. But in terms of just in this initial assessment, if you're by yourself in the field, I wouldn't be pulling out a blood pressure cuff I'd be Checking for pulses. And you're looking for a shock, right? A pulse and shock, do they have low blood pressure because they bled out? Do they have a low blood pressure, because they're in cardiogenic shock, I mean, did they take a around to the chest that may have not hit the heart, but may have nicked the the pericardial sac, which is the sack around the heart, and now they've got what's called a pericardial effusion, which, which is a form of obstructive shock. Now, your heart's fine. But because there's that fluid around your heart, it can effectively pump blood to the system. And there's other reasons to have shock, septic shock, which you probably wouldn't deal with. In trauma. There's Neurogenic shock from you know, spine injuries and things like that. But the big thing is, is pulse and blood pressure, and how do you? How do you fix that? Travis 20:50 Yeah, and I like what you said here, because, like me is really a layperson, it's really cool to hear the way that you talk about really like, the, the difference between when you want to actually use like something like a blood pressure cuff and when you don't, because yeah, like you said, if you just show up on scene, you're treating a patient, you can kind of like, take some of these shortcuts without necessarily having to take the time to pull out a blood pressure cuff and like, take some of these extra steps. So it's really cool to hear kind of like these, I don't know, quicker way of, of making initial assessments, Michael 21:28 it's just a quick way to make that initial assessment, knowing you're going to start to do a secondary assessment, after you kind of addressed all the life threatening, you know, things that could kill someone within minutes. And then as you go on to your secondary assessment, you're going to do a full head to toe, what pressure temperatures, you know, all the other stuff that you could do in a, in a more controlled setting, it's just not important to know what their temperature is right after a trauma. But you know, 30 minutes later, you know, when we're in a safer place where we can, you know, do treatment or, you know, after we've addressed all the, you know, primary things that can kill them, then obviously, we're gonna get all those secondary assessments and things out of the way. So, you know, we've covered the ABCs, and then there's a, d E. So you know, I call it ABCs. But it's ABC, D, E, and then you do your second assessment, and your d is your disability, you know, so why is a person down? You know, obviously, this is like for trauma, you're going to be worried about maybe intracranial bleed head head injury, but if you just come along a person, you know, you're working the residents and someone's just down on the bed, you don't know what happens. It doesn't look like there's any obvious signs of trauma, they they're on the bed, you know, are they hypoglycemic? You know, you've got to glucometer check, blood sugar, did they possibly overdose? You know, you're looking at pupils, are their pupils reactive? Do they have, you know, decrease? respirations? Do you have to give a dose of Narcan? Is there maybe even a history of just opiate use with this with this client that you have? You know, this is all that medical assessments and just kind of knowing who your client is? Is it two in the morning? And they just finished partying? I mean, are they intoxicated, a mixture of both drugs and alcohol? So that's something you could there's a lot of things I mean, hyperglycemia, an opiate overdose, did they have a seizure? Do they have a history of seizures, there's things that you can actually reverse both given glucose and Narcan. You can actually wake up a patient, if that's the reason for being you know, unconscious. And then as you move from disability, now you just go into exposure, you know, are they hypothermic? Are they hyperthermic? Some simple touching of the skin, you don't need a thermometer to know if someone feels like they're burning up? They're burning up, if someone feels cold, they're cold. You know, you don't need a thermometer to tell you that you're just you're just feeling or were they exposed to some kind of chemical or they have in a toxic drum. I mean, are they in the field working, you know, with their gardener, you know, and got exposed to some pesticide and have an organophosphate poisoning and there's probably not much you're going to be able to do if you're, you know, a BLS provider. But if you know that there may have been a chemical exposure, I mean, the first thing you can do is start getting them addressed and hosing them down and just making sure you're safe and you don't get it all over yourself and become victim number two, just simple things. And with this algorithm, if you just kind of know what you're looking for, even in the heat of battle, or you just go on, you know, a before b b before C C before D D before end, just the faster you can move through it, the better but you don't go to B or C unless you've you know, managed a and just think of it that way. And then there's a secondary assessment. It's easy, right? You're just now head to toe. You know, they're awake, they're alert, they're breathing fine. You know, they don't have any circulatory problems and you're checking head and head injuries blood neck, you're looking at their you You know, their throat or they don't have any swelling or injury there, you're looking at the chest, you're touching the chest, you're touching the belly, do you have belly pain? Do you have back pain Do you have, you know, back, lower back, upper back pain, no pelvic use, grab the pelvis, hit it, move their arms, move their legs, look around, and just treat what you need to treat. I mean, hey, listen, you're not in a hurry, and they fell in, they have neck pain, you've got that C collar, put the C call on don't move them. But if it's, you know, you're in a gun battle. And you know, they've got neck pain, and it's safer for you to get the hell out of there. You know, and if they can get up and walk and all they have a seat, you know, see painted, though that call her on and tell him what's what's book, it all kind of depends on on your assessment, you know, at that time, and how, you know, safe that scene is where you're working. It's not your typical domestic, you know, got neck pain, and they're going to be put in a call, or they're going to have a backboard, they're gonna get rolled with three people, you know, maintaining, you know, spinal precautions, so you're not doing any twisting of the torso. Travis 26:04 Yeah, and you raised a really good point here, which is being able to know your patient. So I think in something like high net worth protection, many times you're going to be able to do those initial or initial and then periodic interviews with your principals. So you could understand any underlying health conditions that they have, so that, you know, one, like what are high likelihood and like potentially critical issues that you might run into. And then even in other situations, where maybe a high net worth person is not willing to share any of their medical history, still, you could make a lot of assumptions about their population based on their age by the people around them. And by just like their general lifestyle, so you make an excellent point about knowing your patient and understanding potential medical issues that they might encounter in the future, and those that might be more likely or less likely, based on their age and their lifestyle. Michael 27:07 Yeah, I mean, so I'm in a different situation where, you know, I'm a physician, I'm a medical director, and I've been brought on to a couple, you know, high net worth, private family off security teams. So you've got now a client who's actually actively wanting a physician to train his security personnel for MediCal. So when you get that kind of client, you're gonna get someone who's a little more open. Now, he's going to not probably tell every single person on the team, what medical problems he has, and things like that, because, like anything, everybody's going to be a little secretive about what's going on with them. But you know, the higher level up guys who got the MDS, and you know, some of the guys that are paramedics are going to be trained up for those sorts of things, just knowing full well what the client's medical medical history is. So, you know, I think that's very important just to train on it, to kind of know what to do if a medical emergency arises secondary to one of his medical conditions or her medical conditions. And it's important to know. Travis 28:15 Yeah, excellent points. And I was also curious to ask you, like, Could you speak a little bit about the difference in the level of care that, like a BLS trained person versus and advanced provider might be able to deliver? Michael 28:31 Yeah, I mean, so, you know, it all depends on the state. You know, I can talk about California, I know, well, you know, BLS providers is basically an EMT, basic, right. You know, they're able to provide some medical care, but they're limited in terms of the state of what they can do. So like a biller, the good thing about being an EMT is you you actually get to learn medicine, and you get to learn a lot more than what the state is actually allowing you to do. So, you know, it's nice to have that background even though you're limited, but the reality is, if you're DMT, you could still be very helpful to if there's an advanced provider on your, on your team, on the detail that you're working, you know, and when I say advanced provider, I'm talking about a paramedic, you know, and these medics, BLS provider can do a lot of things, but it's the the medic that can start an IV that can give medications, if a client's got a history of seizure, you know, then there's IV medications we can give or if you're doing a prolonged CPR, instead of just doing your basic, you know, breathing, chest compressions, and that's it. I mean, you're able to give epinephrine you know, if you've got a client that's got asthma, and they're really bad, or you know, anaphylaxis, and you've got epi pens, you know, actually I believe a BLS provider. paramedic can help give an epi pen that they get from the actual patient themselves. So that's, that's helpful. And then they can do paramedics can do advanced airway And they can do sedation prior to airway airway, they can do what's called, you know, RSI, which is called Rapid stands for rapid sequence intubation, and there's paramedics I work with, in the field who, you know, if I'm working, and I've got a medic with me, I don't need to intubate them yet, I let the the medic intubate. Um, I mean, I'm doing intubations on a weekly basis in the emergency department, and they don't get that exposure to as many intubations. And I'm there for backup. And usually they don't need it, it's, you know, pretty simple. And we'll push our side meds and they'll be able to get that. That airway and security and everybody's, you know, good to go. So those are some of the basic, I mean, it's a paramedic, I mean, it's worth their weight in gold in the field, they're used to the field medicine, they've been given the ability to do a lot more advanced medical, you know, but obviously, the cost is paramedic school is, is very long. And, you know, lots of lots of training, but I think even just the EMT, basic, there's a knowledge base that you can gain from going through that training that will make you you know, very, very helpful to advanced providers. And it just gives you opens up your mind when you're doing your security work. Travis 31:15 And one thing that came to mind, as you were talking was epi pens, which is something that is missing from my kit, and, like unique to me, actually, someone that's pretty close to me does have an allergy where, you know, if they come in contact with a certain, like nut, it could impact their airway. So yeah, just listening to you talk, I think that's one thing that I also need to consider, like, as I like, make some changes and add some new things or takeaway of some things from from the medical bag. Michael 31:50 Yeah, so in terms of the epi pen, so I don't think it's a pot, it's it's not on the security provider. If they're a BLS provider to have an epi pen, one, you can't get it. Because it's prescription medicine, to you know, if you do carry it, you'd be carrying it for your client, who was prescribed that EpiPen, probably by their primary care doctor because they actually have, you know, a moderate to high risk of having anaphylaxis. So from previous allergic reactions that may have been, you know, that kind of pre anaphylaxis, and they're worried about the next allergic reaction becoming anaphylaxis, they'd get prescribed an epi pen, but I don't think it's on a security provider to have an epi pen, you know, just in case someone around them has anaphylactic shock. It's the client itself, based on that medical advance for that client, knowing kind of what their issue is, and you know, the clients probably going to be carrying it with them. And also, you know, they may have security personnel on the details, having it or on an advanced, you know, medical kit, you know, in the house or in a vehicle as they're moving, you know, in the city and things like that. So I wouldn't worry too much about having an epi pen for yourself. Unless that said family member, whoever has one in the house or makes one available to you if you're going to be with them. Travis 33:09 Yeah, those are excellent points, and very good things to consider for everyone listening as well. And then next. So moving on, I wanted to ask you, so now as we think about specific emergency medical tasks, can you speak to a few of these big tasks and what gear we should be considering? For example, if we started with, like a patient assessment? Michael 33:34 Yeah. So I mean, I think the patient assessment it's pick one, right, so you're either doing the ABC, D E, with the secondary assessment you're doing, you know, the March pause any of these algorithm algorithms that you're taught, I don't have a preference, whatever you've been taught, I mean, if you're T, Triple C, and you've no March, you know, like the back of your hand, and you do it every two years, stick with March, you know, if you feel like you're missing something for the medical side, maybe, you know, then add it to your algorithm, don't change your algorithm based on Oh, someone taught me this one, or the one you have is the one you stick with, and you practice with and you get fast at it and make it like the back of your hand. And just know what Well, I mean, I can do both, because I kind of know what both of them mean. But I've also been doing it for a long time. So just pick it, practice it and continue to, to go with it. Travis 34:28 Got it. And when it comes to as far as like, tools that we might need when it comes to doing the patient assessment, are there are there like what tools do you think should be like immediately available when it comes to doing a patient assessment? Michael 34:46 Your hands, your eyes, your brain? Those are going to be the you know the first thing and then just as you go through your algorithm, you should have those tools ready right. So your your tourniquet When you're looking at your march pause, if you're looking for massive hemorrhage, your tourniquets shouldn't be in the bottom of your bag, you know, so stack your bag, the way you're going to do your assessments, your tourniquets, your hemostatic gauze, your Israeli bandages, your gloves, so you can do direct pressure, while you're getting all this stuff out. should all be on the outs of your bag, either in your IFAK you're using it for someone else, you're using it for yourself, or your bag, just have them available, and then you're going into airway. So your airways shouldn't be in the bottom of your bag, you know, so plan your bag accordingly. From easiest to hardest to get. And as you're pulling out of your bag, your your tourniquets, and you stop the bleed, then you're moving on to airway and your airway stuff should be there, your MPH should be next year tourniquets, you know, and then just pack your bag accordingly. Because that would is my biggest recommendation. I've seen so many times where it's like, people don't even know where their gear is in their bag. And they're like throwing stuff out of their bag looking for things and know your bag and know well pack it the same way all the time. I mean, unless you're packing it wrong, and you've decided to maybe take my advice to pack the things you need to soon is repack your bag and pack it the same exact way. I think I talked to you or on another podcast about, you know, fine rescue. And I got complacent I didn't check the bag, got a call started looking in the pockets that this stuff was supposed to be in because I wasn't using my bag, I was using the actual team bag. And they had sent out a memo that I missed that they had removed some stuff and moved it into different packets. And we got everything taken care of. But there was delay, not delay that caused any harm to anybody. But there was a delay in me getting stuff. So it was just kind of internally frustrating to myself that I basically just completely dropped the ball got lazy and complacent. And you know something bad could have happened. Thank God nothing did. But it was a reminder to me that complacency. Complacency will kill. Travis 36:57 Yeah, and I love the way that you set it to stack your bag and the order of the items that you're going to need as you do your assessment. Like that's such a simple idea. But as I think about this bag that we're talking about today, yeah, like PPE was available, but is it actually stacked in in like, the most high priority way when it comes to doing those assessments? I think there's definitely a couple changes that I can make. So I do I do love that way of describing it. And so we talked about patient assessment and then could you next share a bit about bleeding control? Michael 37:34 I mean, so I'm gonna oversimplify bleeding control, right? There's three types of bleeding control. You've got torso injuries, you've got extremity injuries, and then you have junctional these junctional injuries are these these weird areas where you really can't put a tourniquet in, you can't really you know, pack, maybe like a torso type wound so you know, your armpits, your groins. You know, let's talk about the simple ones extremity wounds. It's, if it's a massive extremity wound, you're throwing a tourniquet on. If it's let's say, a little five wound cut, that you don't think needs, you know, it's not an arterial bleeding and squirting halfway across the room, you direct pressure and then maybe pack that wound, you pack it in, you throw an Israeli bandage on it or another type gauze or Coban that will cause some pressure on it. And if it's continuing to bleed through, then then you throw a tourniquet on it. You save the tourniquet for what the tourniquets for it's basically going to cause a decrease to no blood flow from the spot that you put it all the way downhill. So if you don't need to put it on, don't if you do do it, don't worry about it. So that basically handles all the extremities, arms and legs. Then you've got your torso injury, so if you've got, you know, an abdominal wound, I mean, if there's bowel coming out, and it's bleeding, you know, push that bowel in, be careful and, and pack that wound or if it's a large thigh wound that you could just get bleeding stop, you know, you're you're packing that wound. And then if it's a junctional bleeder in the groin, you know, you can try to pack it. There's other advanced junctional tourniquets and things that I don't carry. I'm just either going to pack the wound or direct pressure but usually even in those junctional areas you should be able to pack it and you know get the waiting to stop using coal ban. I love coal ban. I carry Cauvin with me it's just basically like a like stretchy gauze that just sticks on itself. It's just great. It's like not as sticky as duct tape but it's more flexible than duct tape so you can kind of pull it even more tight to get direct pressure on things and I love this stuff. So that's basically my Mikey's the bleeding control, I mean, and then there's just other internal bleeding that you just aren't going to be able to stop. I mean, if someone has, you know, penetrating injury and it's hit a large vessel on the inside of their abdomen, there's not much you can do other than just get him to a trauma center. You know, there's some advanced stuff, I carry TSA, which is using the military, I can give it you know, even in the county, I work in paramedics are allowed during trauma under certain conditions to give TX A in the field on the way to a trauma center. So if you've got a medical director, and you've got a paramedic, and you're going to be in a, you know, possibly high risk, so like in the city, probably not going to be giving TSA to someone who may have gotten in a car accident, or something, if the trauma centers five minutes down the road. But if you're in rural Montana, and something happens, you're out biking, and you know, you're now hypotensive. And there's some signs of internal bleeding. You know, that's would be a great medicine for advanced provider to have while getting to a trauma center. Travis 41:01 Can you share a little bit more about what TSA is and how it works? Michael 41:06 So, yeah, I can get into the mech. And I don't know if you really want me to get into the Travis 41:10 like, like, not not too deep, but like, is this pill? Is it something that you place on a wound? What is it Michael 41:18 Yeah, so TX A is actually it's a bio of liquid medication that's given intravenous intravenously. And what it does is it just initiates the clotting cascade. So for these internal injuries, it basically just helps you clot. So the, the wound so you would never give it if you only had an extremity injury, let's say someone severed their arm and you're able to, let's just say you took your whole arm off. And that's all it was, they put their hand through a grinder, and you're able to put a tourniquet on there, you would never give TSA, it's more for the internal injury, torso bleed, abdominal bleed, pelvic bleed, that you can't access, you can't stop that you would give it for and it just increases the clotting cascade to to start you clotting internally. So you don't continue to bleed out. Travis 42:11 I see. Okay, yeah, I was just interested. But it's all Michael 42:15 it's not something you're you're not going to get it over the counter, it's a prescription medication, it has to be an advanced provider. That's giving it and you have to stick to, you know, strict protocols on how you're given it, you don't want to give it willy nilly, you don't want to give it to some, you know, cut his finger and you're given TSA, that's just not, it's not what is before. Travis 42:34 Yeah, and that definitely highlights the need for for those people that are for those high net worth people who are traveling to like these more austere or like rural type places, the need for having a medical medical director and for having someone that could deliver advanced care, not just someone like me, who went to an EMT course and took a couple of seminars, so that that makes total sense. Michael 42:57 It's, it's a medication that's basically stolen from the military, it was something that the military has been using forever and forever and forever. And we finally domestically have have used it. And I've gotten my own reasons, probably why I think it's probably because it's a very cheap medication. And you know, sometimes the medical complex doesn't want to use cheap medications. But I think there's so much benefit to it with as many traumatic injuries that we have in the States, especially with, you know, these med flights and where people are rural. And they're getting into these injuries, these accidents that we have to start using domestically. And we're starting to Travis 43:34 interesting. And next. So I wanted to continue over to another topic, which was I just wanted to ask you like, what, what else do you find that many people overlook when they're putting together their medical kits, or they're just preparing, preparing their their knowledge of Emergency Medicine? What do people tend to overlook in your experience? Michael 43:59 So I think one thing is because a lot of this medical equipment is expensive, sometimes they want to get some knockoff stuff. I mean, the tourniquet is 40 $45. There's some of these knockoffs you can find on the internet for 10 bucks, I would just, you know, I would stay away from those things. You just don't know how well they're made. You know, if they're even going to work, it's not something you want to practice, you know, your tourniquet that you're going to use, you probably don't want to use that to practice. You know, maybe use it one time to make sure there's nothing wrong with it. But after that you're done. You know, you have practice tourniquets. Maybe having stuff that you're just not going to use, like if you're not supposed to be doing a needle thoracotomy you shouldn't be carrying a needle. You shouldn't be doing something that you're just not fully trained to do. And just carry it just in case. I think those are probably the two things that I can that I can think of. Just carry what what you're range use and you know how to use? Travis 45:04 Yeah. And then what about, um, can you speak a little bit to, like, the benefits of conducting a medical advance and knowing the area that you're going to be operating in? Michael 45:18 I mean, I mean, that's the way I see why I'm brought on to some of these teams is, is, is doing those medical advances, right, just to think, you know, way outside the box and figure out, you know, what's the client's medical issues? You know, what about the Friends of clients don't move by themselves, they usually move with family, friends, on vacations, they go international, they, they, they travel, they move. So you know, even the family and the medical conditions, you know, for my clients, I know about what's going on with all the siblings, and kids have siblings and things like that. And we train and, you know, bring equipment accordingly. And then just using that information to train up your, your personnel, I mean, if a kid has got a medical issue, and you train up on that medical issue, how to do the dosing of the medications for a specific age and size, a lot of Pediatrics is all size based dosing of medications, and then making sure that you bring the appropriate equipment with you and appropriate medications with you, and that you haven't enough if the, if the client, you know, misplaces, his blood pressure medication, do we have backup? Do we have access to a facility where we can get more medications? Depending on where we're going? Do we need to find a local doctor to get that prescription? Or is it just easier for us to bring extra medication? In terms of like, doing the advanced is? Where are you going? Are there hospitals near? Do you have trauma centers? Do you have pediatric centers? Do you have a way to get to a trauma center? Do they have an EMS system? Is the EMS system? 24/7? Is that a volunteer system? What's the what's the transport time during traffic non traffic times? What's their ability to get to you in a timely fashion? Is it a, you know, five minute response time? Or is it a 30 minute response time? And then also, the big thing is, is telemedicine telemedicine capability? Do you have something set up? Where if something does happen? Let's say you don't have an advanced provider? Do you have the ability to get on the phone with a telemedicine provider in your area in your country? In the country you're going to be? Or do you have a medical director that you can call or maybe someone on your team as a medic that you could get advice from if something were to happen, and they're not, you know, on the trip, and then all the way up to the evacuation plan? You know, depending on where you are, do you have the ability to get to, you know, if you're in a third world country, maybe they don't have advanced medical to get to, you know, back to the States or to another country that has a more modern health health care facility? And have you set up those details in advance instead of trying to do it last minute trying to find a air transport provider? Or, you know, how do you get off so and so Island to you know, United States, like from the Caribbean to Miami? How are you going to do that? Can you do that via helicopter? Do you need a plane? Do you need to transport plane, you know, so all the things people don't kind of think of because it's out of their wheelhouse. It's it's not security based medical advanced, more of a medical advanced is where you get, you know, your your paramedics and up and you know, that can kind of think way outside the box and plan for everything that could possibly happen. Travis 48:45 Yeah, and listening to you talk about this, it just shows so much how, yeah, when you're doing a lot of security tests, preparation is everything. But also there's so much involved on the medical side, when it comes to conducting an advanced prior to going to like going out of the country. So I think those are some really interesting considerations. Yeah, well, Michael 49:09 one of the considerations is when you're actually talking with some of these air transport companies, they may not let your security personnel or family on the helicopter or plane. So that's something you have to discuss, you know, if you've got ultra high net worth individual who's now being transported from, you know, a country into the states, and now they're gonna have no security with them, or family members, that may not be something that the you know, client is going to be happy with. So that's also something you need to get maybe in writing from the air transport personnel say, Listen, you know, we need to bring someone so with us, you know, during transport. Are you guys good with that and making sure that, you know, that doesn't become an issue. Travis 49:51 Yeah, that's a really good thing to think about too. Because like, yeah, we have to think through all these worst case scenarios and how how Logistics is going to work out in all them and then also going, like right back down to the human element of yet. How was the How was the principal, how's the high net worth person going to feel if we have to do X or if we have to do Y and they can't be with a security person. So yeah, that's, that's an excellent consideration. And now, so I wanted to for the last part of the podcast, I want to see if we could do kind of like a general walkthrough of some of the items that we have in the bag. And this could be more like a rapid fire round, because we could probably easily spend a few hours talking about some of the advantages and disadvantages of different items or what I was missing or why I have so many of x instead of y. So Is it cool if we do like a walkthrough of some of these items? Michael 50:49 Sure. And you already sent me the items, obviously. And it's I preface it by it's all scenario based, right? So there's going to be some stuff. I mean, I think all the stuff you carry is great. I may think that maybe some of that stuff, you don't need to hold on your back, all the extra weight and just space. But it would be great to have in the vehicle, maybe left in the vehicle. But I just kind of preface it. So I don't want to sound like I'm nitpicky, I just kind of preface it based on you know, what, what, what would you know, how are we going to discuss this? What's your role? why you'd be carrying this bag? You know, what's your mission? Travis 51:25 Right? Yeah, so really, the purpose of the bag is kind of just, it's almost like a catch all bag. So like, if I'm not around. If I'm not around a completely decked out medical bag, this is something that I could just throw my back, throw in a vehicle and just be able to provide like a minimum level of emergency care. So that's, that's really the main the main point of it. Okay, got it. Yeah. So if we start with the first part, which is like some of the outer pouches, are there any? Are there any things that stuck out to you as maybe good or bad? Michael 52:05 So I think the SAM splint is great. The SWAT tourniquet. So my only issue with the SWAT tourniquet it's not great for one handed application. So if you're carrying a SWAT tourniquet and you have to put it on yourself, it's not really that great. If you're putting it on someone else wonderful. If you're putting it on a child, you know, even better, depending on how big the child is, if the child is very small, then I think the SWAT is perfect. You know, your, the blast bandage that you had, I think it's great. You know, it's it's personal preference. But you know, people can use God's cope and kerlix altogether doesn't have to be a package blast bandage. Krazy Glue, I would if you're able to get Derma bond, which is medical grade. I think that's even better, because that's something if you have a small cut that you can clean you can you know, repair pretty quick. splinter out Sharpie pens, Gorilla Tape, electrical tape, I like duct tape. I mean, I I think electrical tape, gorilla tape all that stuff. Duct tape works just as well. It's going to be preference splinter out? You know, I don't know, I think that's probably just overkill. I don't think anybody can just wait till they get home to get splinters out, you know, carrying a Sharpie pens. Yeah. I mean, you should have probably a Sharpie and a pen on you, on your person. You want to go through? Travis 53:26 Yeah, and you make an excellent point. Like, I think some of these items were more like, I don't know, they were just like, easy to throw in the kit. And I figured they could be useful. But yeah, you make a great point, like, do I in the emergency kit? Do I need to something to take out splinters? Like, honestly, like tweezers would probably work just as good and be useful in other circumstances. So that's a that's a good call out. Michael 53:50 It's just preference. I mean, if you don't mind carrying it, and every time you go out and double checking that it's it, because my thing is you should have an itemized list of what's in your bag. Because it's real easy to go. Yeah, my bag looks fine. And once you're actually doing a checklist, you're gonna miss some. Travis 54:07 Yeah, that's an excellent point, too, of having an itemized list with the bags of you know, what's there, what's not there? And you can assess it. That's that's a great point. And let's see next, can we move on to the secondary container? Michael 54:22 Yeah, so on the secondary, you've got this Eric care patient assessment for him. I think that's great for a patient handoff, you do medical care, they know exactly what you're, what you've done, kind of your assessment and some changes in the habit, the MS field guide. So that's something that I think if you can get web based, you know, on your phone downloaded on your phone, I think that would be better. I think the other thing is it's just an optics thing, right? Last thing you want to do is your client sitting there and you pull out a field guide. It's just gives the optics like maybe you don't know what you're doing. And this is from a person who thinks I'm a strong proponent of checklist Just like, you know, I'm a pilot, and everything is a checklist as a pilot, but somehow when you go into medicine, there's no checklist. So you can run, you know code, and you're just doing it from memory with, you know, adrenaline rush in, you know, lots of noise, lots of why there's why we're not using checklists in the hospital of like, you know, CPR and what you're supposed to do with the time and the minutes. For me just being an air plane and knowing that when I get into the plane, before I get into the plane, I'm doing a checklist of you know, all the the plane and making sure everything is fine checking oil, fuel, what have you smelling fuel, looking at the fuel, making sure it's not contaminated, getting into the plane checklist to turn it on to turn it off, checklist. Taxi, you got a checklist to do everything. And I think in the medical field when you're dealing with life and death, doing CPR and advanced things, why you wouldn't have a checklist is kind of crazy to me, but I think it's just that medical. You know, that machismo like, Oh, I'm a doctor. I, I you know, I know this stuff. But the reality is, is probably in every code, there's something that was done wrong, not done in the correct timing, time was delayed or something. But anyway, that I'm digressing but I think the field guide is is a little much if you could have it on your phone, that would be better and it's just less weight that you got to carry in your in your back. I think multi tools great moleskin it's kind of the same thing as you know, the splinter out you know, I don't know carried if you want I don't know if it's really emergent Kleenex travel pack. That's just what Kleenex Travis 56:36 Yeah, just Kleenex. Yeah, just Michael 56:37 Kleenex. Great, wonderful. One another one of these things you have a you have it all depends on your mission. Right? NPAs and OPA I think you should at least have an NPA. Be careful with trauma if there's any kind of high risk of possible head injury. Or if you've got clear fluid, which would be possibly CSF, you wouldn't want to put an NPA Be careful with putting an OPA because if you put an OPA in someone and they got a gag, you may use vomiting, you may induce all kinds of problems. A Spanish I think is great. I like Cauvin. You know, if you've got four by fours, and you've got Kobe that you can wrap around, I think you just get a better tighter seal. But I think ace bandage along with CO BAM would be perfect. And then you know, we have this discussion offline in terms of your over the counter medications. So I know you mentioned that you had a couple medications in there that you weren't even sure what they were. Yeah. So that's where I think, you know, I mentioned earlier the the list, having a checklist. So if you knew all the medications that you were carrying, you could just by default, realize oh, well I've got Imodium. I've got Benadryl I've got Advil, etc. And baby aspirin, Oh, I must be missing Tylenol. So one of these pills or Tylenol, to prevent all of that. I would just take you know they've got these factory package medications where you can get baby aspirins and the little you know tearaway baby aspirin pouch and Excedrin and the Advil and things like that. I think one medication that you probably should is Pepcid. You know, it's some over the counter for antacid. Pepcid. My favorite thing for anybody who's got reflux, and it is a high sodium load. So you have to be careful. Like if you got a patient or a client who's got congestive heart failure, or who has some kind of sodium limit on amount of sodium, they're supposed to have baking soda, a quarter teaspoon of baking soda, eight ounces of water. If you've got, you know, indigestion, you know that baking soda is so basic, it just counteracts the acidity in your stomach, and it usually makes people feel better. That being said, you know, you got to you're not playing doctor there. It's you got to ask the client this I have this, you know, you want to try it. So I think that is, you know, for the secondary counter a container. It looks good. I mean, there's just things that I think are probably don't need, but it's all preference, if you're willing to carry it, and you're willing to you know, inventory it and make sure you have it every time then I say go for it. Travis 59:26 All right. Awesome. Yeah, those are some excellent suggestions. And yeah, I will definitely, I will definitely consider the tiny individually wrapped packages for the medicine. That is, that's an excellent suggestion. And then next, so we have the main container, starting with our red trauma pouch. Michael 59:46 So the Trump pouch you've got the hemostatic gauze, I don't particularly have a preference. The chest seals so you do have to so it's always nice to have two chest seals, right because of traumatic injury. You're usually going to have an entrance In exit, you may just have an entrance only, but for every hole, there should be a chest seal on it, you're gonna have scissors, shears, you're gonna have gloves, I'm hoping you have another pair of gloves in your outer pouches or on your person. So if you have an extra pair, that's great, but if your gloves are in the red trauma pouch in the bottom part of your bag, you know, that's a no go for me gotta have it, you know, on your person or on an outer pouch very easily accessible. And then wrapped material. So for me, like I said, I love Cauvin, you can use kerlix Ace wrap, you can use your Israeli bandage as you know, some kind of wrap material. Also, if you start to run out, you know you have a C spine. I don't know if I would want to carry C spine color is it's big, doesn't weigh a lot weighs ounces, but it's just bulky, I would say keep that in the car kit. And the reality is if something were to happen, and you do need a cervical collar, there's probably going to be some other injury and you're going to probably need a backboard. So the reality of you have an A C spine, collar and moving the patient without a backboard, it's just like, that stuff could stay in the car, you know, you could probably manually just hold their holder neck and help them just remind them to not move until you can get them stabilized BVM. So I was already gonna, I Travis 1:01:24 was gonna say that that's an excellent point. Because that's something I hadn't considered. I thought, Oh, we could just throw C spy on him. But you make a great point, which is that you'll most likely also need a backboard. So having just the C spine, and plus a does take up a lot of room in the bag. So yeah, great, great point there. Michael 1:01:41 Yeah, I'm gonna, I'll probably tell you out of your whole bag, that was a thing that I really care to see. Because it's just, it's just big and bulky. And then if you need something like that, the mechanism is probably going to be, you know, another multi injury and you're probably moving the patient on a backboard. So I think that's probably something you can, you know, keep in, you know, a vehicle med kit, or at home or at a residence move moving along. So you've got to BVM you've got one of these compact BVM I think that's great, you could carry even some smaller like a CPR mouthguard with as the one way valve. You know, depending on who your client is, it probably depend on who the client is, I don't know. You know, in terms of their lifestyle and things, you want to be careful how high risk they could be for you know, if they're big partiers and, you know, using drugs and things like that, I don't know, if I want to put my I'd rather just have a BVM we'll just keep it at that. Eye protection. So you know, you've got extra eye protection, or most people are wearing sunglasses, if you have the ability to if you have to do medical care, have clear glasses, in case you're in a dark room, you're not going to probably be doing work with sunglasses just have a backup pair of you know, safety clear glasses, so you can see what you're doing. Through forehead thermometer. It's another thing it's one I don't think they're that accurate. We use them in the hospital. And it's the bane of my existence is when they do these thermometers. And the temperature is off by two degrees. You know, you get a kid that they say is got a 99.1 temp, you feel the kid and you're like, can you guys do like a rectal, oral, you know, temp and the kids got 103 temp, they're just not that accurate? I think it's probably not that necessary to have in a field kit. If they're hypothermic hypothermic, you're probably going to want to go home, you're not going to feel that well, you're going to the hospital. So that's, you know, plus or minus people like you can have a pupil light there's, you know, to save space, there's lots of pin lights that have lights on the tip where it's a pen and a pupil light. Worst case is you've got your phone right your phone's got a flashlight. In the hospital, we'll see patients in the in the waiting room and if I have to look at lights, you know, in their eyes or in their throat, I just bring my phone, boom, boom boom versus trying to walk back to the office to go grab, you know, otoscope ophthalmoscope phone works just as fine. And then you've got your glycine pouch. Perfect. So, you know if your clients not diabetic, you probably don't really need it. Your most people who aren't diabetic who aren't taking diabetic diabetes medications, or fasting probably aren't going to be hypoglycemic. So I don't know if that's really necessary. But you do have oral glucose if you don't have or glucose you can just sugar packets, you know if someone's kind of low and but they're still awake and alert and give them a soda candy bar, don't give them diet soda, please. I've had patients come in where they're like, oh, yeah, my sugar was low and I drink the Diet Coke. And I'm like, well, that's not really sugar. That's not going to really do much. But people just don't think that far ahead. You'd be surprised people don't think that far ahead. Like diet. Soda has no sugar, so don't drink soda if it's diet, not going to help you. Anyway, so you've got to test in, you know with the reader and then the extra stripped so, you know, I think that's also something for me, I carry it. If my client wasn't a diabetic, I probably wouldn't carry it, I wouldn't want to deal with it, they're expensive. You know, the test strips are expensive. If you're not using them, it's just kind of a big waste. Stethoscope blood pressure cuff, I carry him. That's a that's a plus or minus, I don't know, if you, depending on what your situation is, what the advance is, what the threat is. If you've got room carry him, if you know how to use them carry him. I mean, it's really hard to do a manual blood pressure cuff on the street. A lot of times, you're just doing it by pulses only, you have to listen to the radio, you know, there's noise or street noise. And a lot of times they'll just get you know, blood pressure 100 overpowered because they can't hear. And if you don't know how to use it, there's no point in bringing it with us. I know. It's It's fancy and all but you know, some sometimes these automatic blood pressure cuffs are better, because you don't have to listen to it and you can you can put it on and do other things. And you don't have to waste 30 seconds trying to listen for it. So I would recommend if you're gonna have a blood pressure cuff is have an automated automatic blood pressure cuff. Travis 1:06:16 Yeah, that's an excellent point. And that's something I'll definitely consider incorporating. Michael 1:06:21 And then so you got kind of the miscellaneous band aids, antiseptic, sterile saline, triangle, bat and triangle bandages. Fine. If you want to carry that it's nice to have. And then the RED camera I thought was good. And I'm not sure why you picked the red. Was there a specific reason why you had the red cam lit. Travis 1:06:40 I figured just something to use, like during nighttime, like something for extra light, extra light or even just like to maybe mark an area maybe something happens and you worried like traffic is going to be coming by or something. Michael 1:06:54 Right? Yeah, I mean, I think right, it's perfect. You know, it's great for night vision. So it's the middle of the night you've got a red light versus just a bright you know, flashlight. We're just gonna screw up your vision, the patient's vision, I think red is perfect. When I fly at night, I've got you know, a red lip light and a red light that I can use in the cockpit. And it doesn't affect your, your night vision. So I liked that you you chose red eye care box. So you've got you know, cleaning solution, iPads, wash cup gauze adhesive strips, I would use paper tape, if you're going to use any kind of adhesive on the face. The paper tape is just easier to come off versus that plastic tape. It's painful, it hurts. For me, I carried prepare cane which is a topical anesthetic. So anybody who's had a corneal abrasion or ever had eye surgery, where they, you know, LASIK or LASIK surgery, I mean, it feels like there's sand in your eye, if you have an abrasion and it's the worst pain for two days. Plus, you just add a drop of pear cane and you go from your I can't even open it to that sensation of sandpaper to like filling nothing. If you can carry that stuff. Carry it. And I suppose you use it a ton. Because if you use it too much it can affect the eye but for, you know, maybe use for six hours that you can get to a hospital and get medications and things, that stuff is worth its weight in gold. So I think that's it in terms of your back. I mean, I think it's a overall it's a great bag, there's some recommendations and some changes, I think, like I said, the blood pressure cuff, the C spine, you know, some of the other smaller splinter off and things like that. But otherwise, I mean, it's it's a good setup, you know, fix your medication issue that you have, in terms of just kind of having them labeled and things. The one thing I will add is if you do find yourself in a rut somewhere, let's say you're out in the middle of nowhere with your client, you realize hope, man, I forgot what medication is what because I didn't label it. There's a program you can put on your phone. It's called epoch parties. And it has a pill ID finder. And so you just basically open up your phone and it'll ask you the rules like or ask you basically what the pill is. It was basically asking, you know, is there a code on one of the sites? I mean, a lot of these pills have numbers on them. What kind of shape is it? Is it oblong? Is it circular? Is it oval? What color is pink, yellow, white? And then it'll ask you if there's any scoring is there like a CT scoring where it's across where you know, each pill is cut into quarters, it is cut in half? Is it like a partial score? And you can actually, you know, usually find out what medication you know it is by just that if you don't have the name of it, some to have hopefully you don't have to use it. I use it for you know, patient comes in. And so yeah, I took a bunch of these and they don't have it in anything and you got to try to find out, you know what the what the medication is. But in the field, if you do find yourself in a rut, then you can use that. Travis 1:09:51 Yeah, that's a really cool idea. So I will definitely link to that within the show notes. Also, I think another thing that I will include in the show notes is kind of law Like, maybe like my top five or my top 10 things that I'm likely to change based on like this chat. So I think people, people could have a little bit of an idea of like before and after. So I think that'll also be really useful for people to check out in the show notes as well. Are there any other ideas or topics that were top of mind that you wanted to talk about before we close out the show? Michael 1:10:30 One other thing, just kind of going through your bag, I think there was a couple recommendations in terms of what you didn't have in the bag. I think one thing to consider and adding is a second tourniquet, and I like what it's called a rat's tourniquet. So if you're looking for a second type tourniquet, let's say you already have a soft T or a windless type tourniquet, maybe just use a different type. And it's a rat's tourniquet. It's basically it's almost like a figure of eight metal strapped to a large cord. And, you know, obviously, you should be trained in how to use it. But it's something that like on a cove protein, you could just wrap around your waist as a belt or a secondary belt. So that if you ever needed access to the tourniquet, you have probably one in your eye fact if you're but it's just very concealed concealable. And as basically no extra weight on your on your hips. And it's a great tourniquet to use. And then, you know, if you decide not to use that rest, you just have a second backup somewhere. So, you know, you're carrying a SWAT, if you have a windlass type tourniquet, like your soft T, there's some ratchet type tourniquets, whatever you train with, I would just try to have a backup and that would be my my other thing is just to have that backup. Travis 1:11:49 Yeah, that's a that's a great point. And that was one that was supposed to be in there, but it was in my truck. So yeah, that gets back to me knowing my gear. Michael 1:11:57 Yeah, it's knowing your gear. But also, if you're in a, let's say, you're doing a cove protection, and you've got two people, three people, four people on that on that team. If everybody's carrying a tourniquet, you're probably going to be okay, because obviously, you're all going to converge on, you know, your your client and try to evacuate, but you guys are going to be with each other. So you'll have backup gear also, which is which is also nice. Travis 1:12:22 That's a good point. Yeah, so Michael, I really appreciate you sharing your time with me today. So I took away some really good ideas like everything from stacking my bag in the order of the items that I'm going to use when I'm doing a patient assessment. And I'm, and I come up on a real emergency. And then also really just kind of like, having another way to think about my bag. So I think you might have phrased it in the way of like something like in an act like in a critical situation are you going to need x item like the splinter out like the moleskin, like some of these other items that can kind of be transferred into a second bag and maybe just sit in the vehicle so that they're not taking up too much space in the primary bag. So you also kind of gave me some other ways of thinking about the gear that goes in the bag, how it's packed, and really like, yeah, really how it's packed so that it can be accessed quickly in any emergency situation. And, of course, all this information will be within the show notes. So everyone after the show or during the show, go check it out, you could see a list of big ideas from the show of the pictures and the itemized list of all the gear that we were talking about today. And then also some useful links. So Michael, I really appreciate you sharing your time with me today. I know this was some really cool information for me and then also for listeners. So I'm super grateful. Michael 1:13:55 Appreciate it once again, Travis for having me on hopefully, like, you know, previous podcasts this information is helpful to people maybe helps them think a little more out of the box in terms of you know, carry medical gear not being so worried that this is you know, above their pay grade. I mean, I think everybody should learn it. And with time, you just get used to it and it becomes second nature to you. And, you know, it's just an extra skill that you have for your own personal home life and, and you know, and for your client and you know, to help you in your career. Travis 1:14:29 Thank you. And I know people will take away some big nuggets of wisdom from this. So thanks a lot. Michael 1:14:34 I appreciate it. Thank you, Travis.


